Right-Sizing the Community Hospital: Optimizing for the Future
As U.S. health systems prepare for an uncertain future, our prototype hospital looks to expand care with fewer beds.

The U.S. healthcare industry is in crisis. Rising costs and diminishing returns are leading to hospital closures and leaving many without care. The health effects of climate change are straining the system, while our communities are demanding health equity. In 2024, the federal government spent $1.9 trillion on health care programs and services, but as the administration looks to reduce spending, future funding is uncertain.
Meanwhile, our population is shifting, aging, and ailing. Parts of the South and West are seeing rapid growth, while parts of the North are shrinking. The “age wave” is upon us, with an influx of older adults and the extended healthcare needs of a longer life. Adult health is declining, with 42% of Americans suffering two or more chronic conditions, and the care they require is increasingly complex.
These dynamics are leaving some health systems without the patient volume to support existing hospitals, and others bursting at the seams. The U.S. has more than enough beds, but they’re not in the right place, existing infrastructure is aging, and there are too few beds supporting critical care.
Whether health systems are planning for growth, consolidation, or modernization, all face questions about an uncertain financial and regulatory future and how to do more with less.
Gensler’s healthcare practice, alongside engineering partners BR+A and Thornton Tomasetti, have designed a prototype to illustrate how financial, environmental, and experiential goals can align to expand community health. We call this prototype Horizon.
Horizon proposes a shift from the traditional community hospital to smaller, more specialized facilities focused on critical and high-risk care.
Here’s how Horizon is right-sized and optimized for the future:
Right-Sized
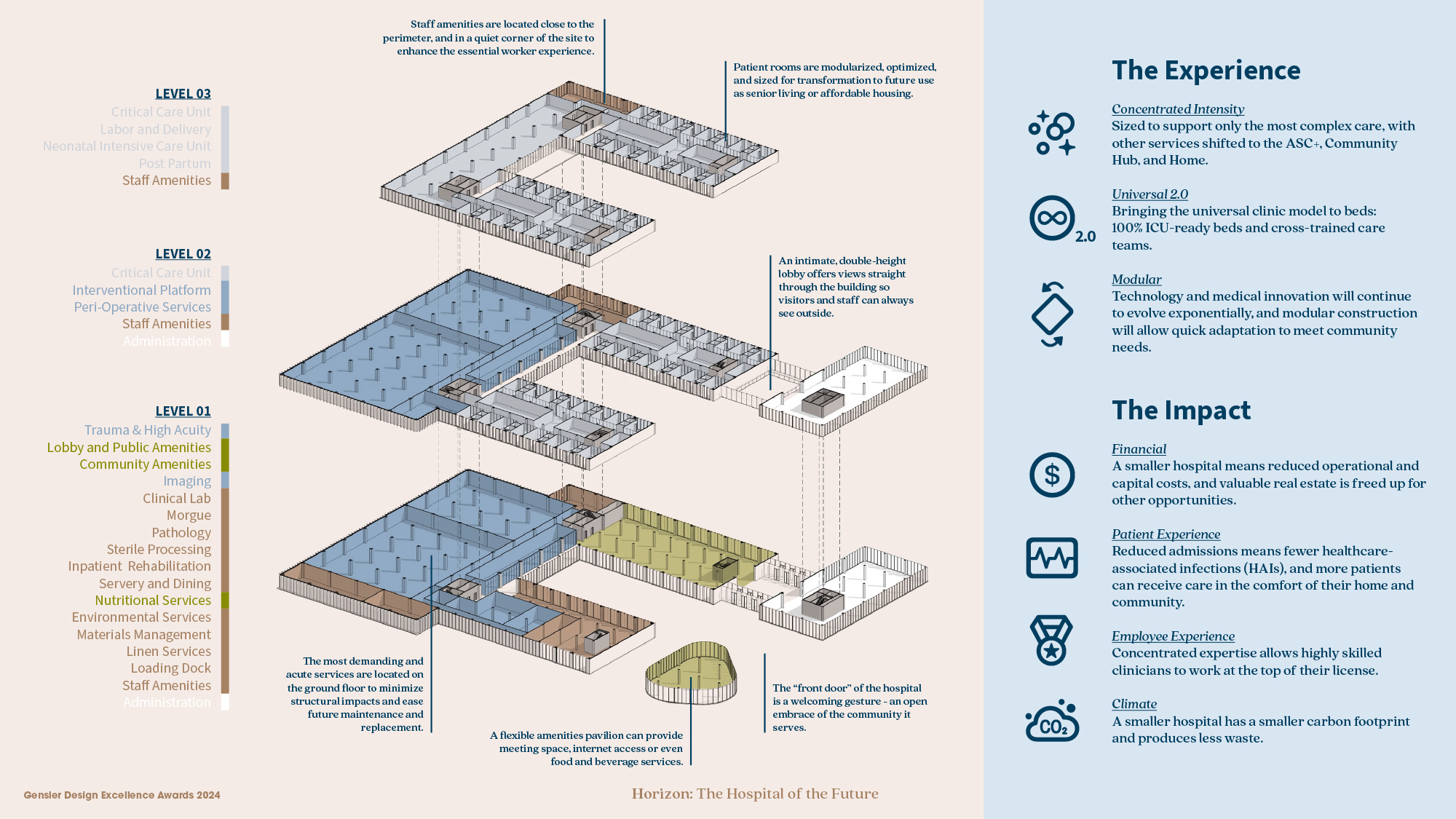
Designed to provide only the most complex care, Horizon is 30-50% smaller than the average community hospital. All but the most high-risk procedures shift to advanced ambulatory care centers, which can utilize existing buildings to reduce capital expenditure and climate impact, and support services are consolidated into logistics hubs for improved system-level efficiency.
Community hospitals today range in size, with an average of 129 beds, of which only 12.2% are dedicated to critical care. Despite the growth of Ambulatory Surgery Centers (ASCs), nearly half of hospital-based procedures are outpatient. Horizon includes far fewer beds and procedure rooms than an average community hospital, with a focus on critical care, high-risk procedures, and trauma care. Stable acute and post-acute care largely moves into lower-cost residential settings by leveraging hospital at home and hybrid programs.
Focusing on the most complex care allows for a more compact, efficient, and purpose-built facility. Horizon is smaller, more porous, and more approachable, seamlessly woven into the urban fabric and a central resource for the community it serves.
Optimized
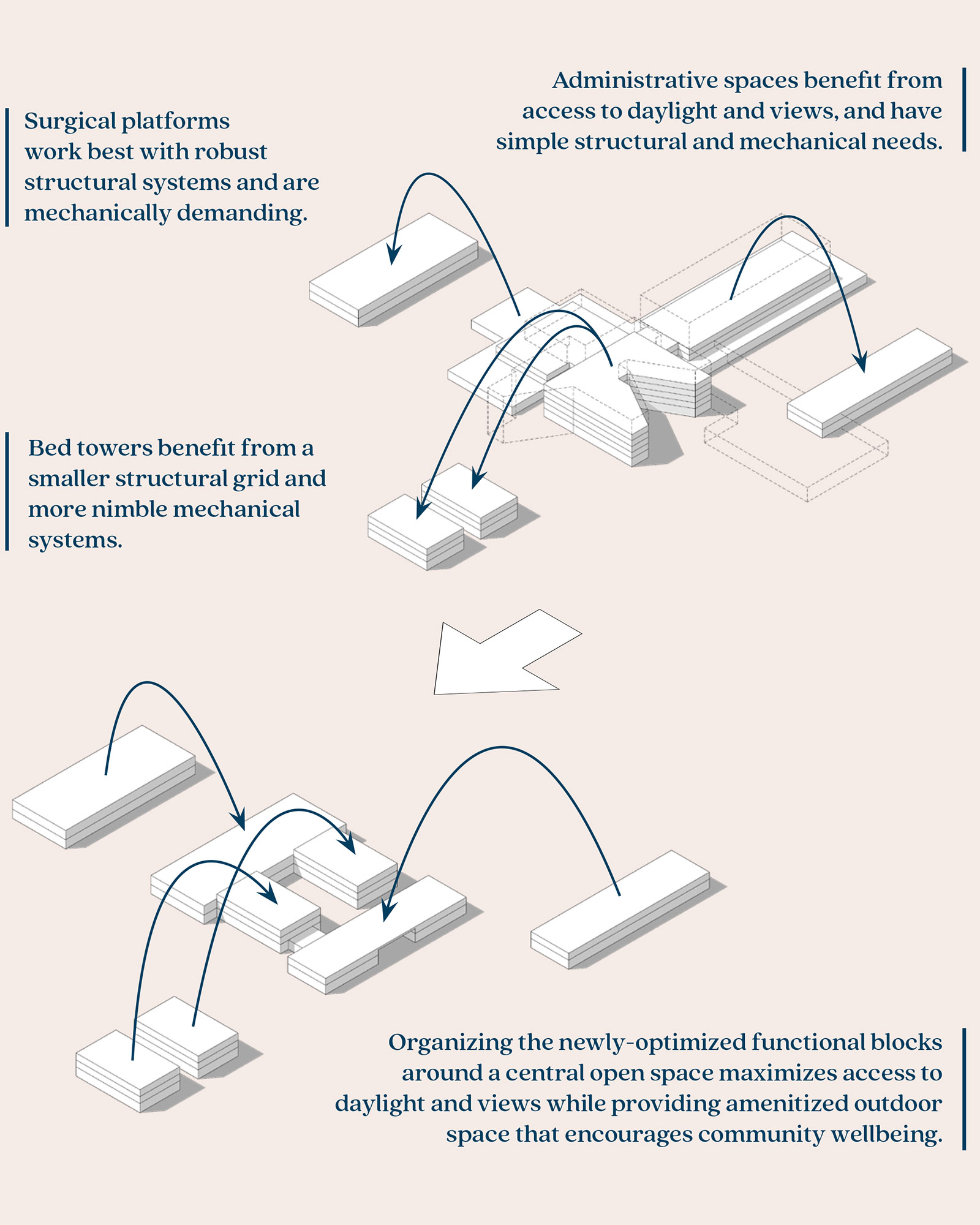
For the last century, we’ve built our hospitals by stacking disparate programs — parking, emergency departments, surgical platforms, administrative suites, and bed towers — atop another. When we could no longer expand upward, we began to sprawl outward. The most important functions of the hospital ended up buried in the center, farthest from the people who needed them most. These increasingly specialized designs and vertical stacking of program have resulted in a steady decrease in useful life.
The right-sized hospital of the future offers an opportunity to rethink these critical adjacencies, and to fine-tune each so they can operate most efficiently.
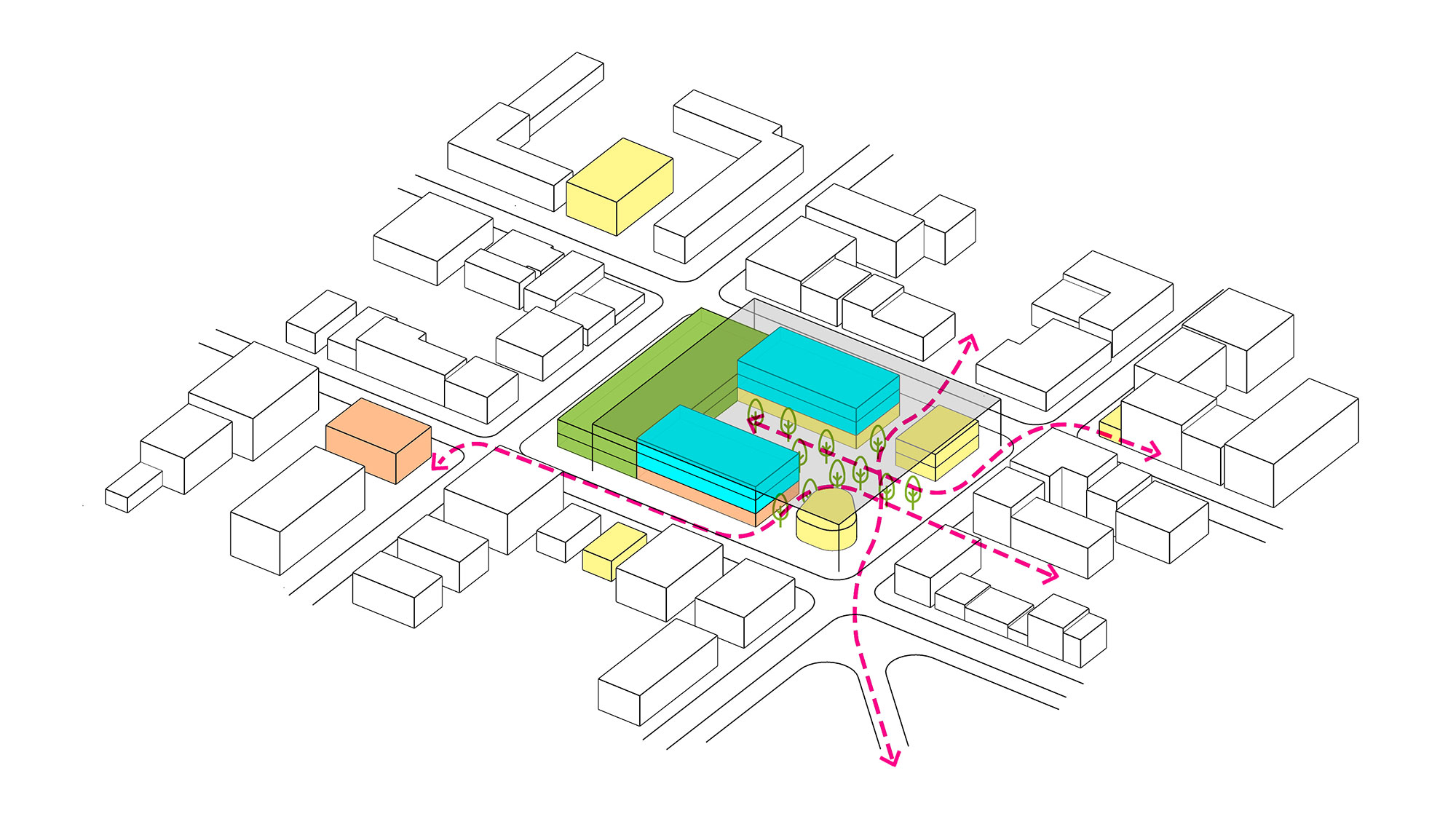
Horizon’s U-shaped form enables long-term adaptability, with inpatient wings designed for conversion into other compatible uses at the end of their useful life as a hospital. A deliberate approach to programmatic organization allows for optimization. Horizon is optimized for current use-cases while remaining flexible enough to adapt to other space-types as needs evolve.
Right-sizing and optimizing the critical care hospital has numerous benefits economic, environmental, and social benefits. A smaller hospital means reduced operational and capital costs, and valuable real estate is freed up for other opportunities. Reduced admissions mean that highly skilled clinicians can focus their work at the top of their license and more patients can receive care in the comfort of their home and community.
This ecosystem approach integrates and redistributes health and care services to focus care in the community and on the patient to provide the right service, in the right place, at the right time.
The regulatory landscape is in flux. The future is uncertain, but we remain hopeful that funding, coverage, and reimbursements will support new models of care delivery that lower the capital burden on health systems and provide alternative options for quality care and an enhanced patient experience.
For media inquiries, email .









