Why Resilience Planning Is Crucial to Safeguard Health Systems
Investing in proactive resilience planning, rather than reacting to extreme weather and climate disasters as they unfold, will help ensure uninterrupted, quality care.

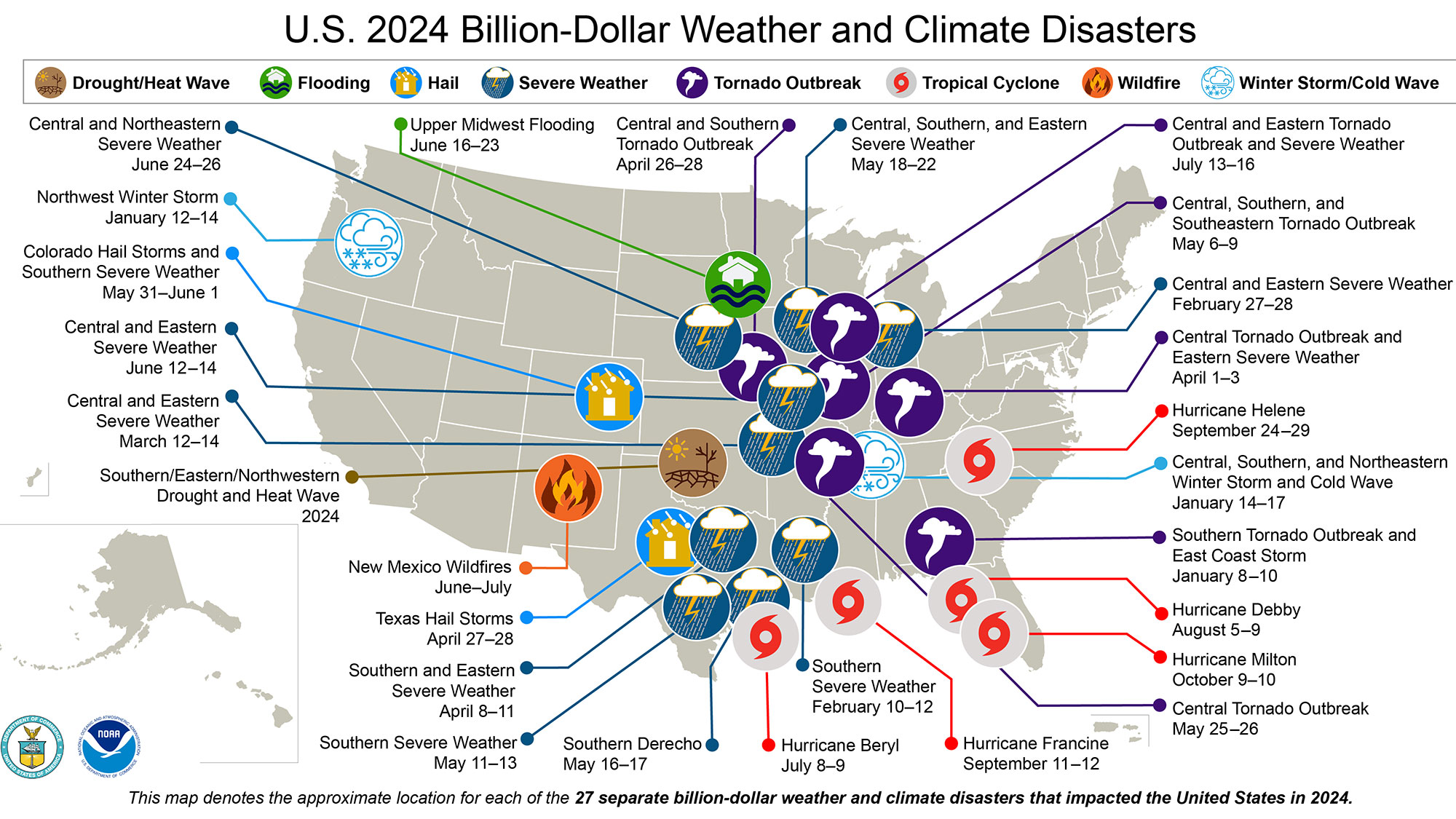
Delivering exceptional patient care means staying operational and accessible, even amid unpredictable weather events. In 2024, the nation experienced 27 confirmed weather and climate disasters with losses exceeding $1 billion each. In total, the United States confirmed that 403 weather and climate disasters cost more than $182.7 billion, per National Centers for Environmental Information (NCEI).
In these evolving conditions, we must move beyond traditional design and construction methods to address the needs of patients, caregivers, and staff. In doing so, a health system can uphold its commitment to the community and its duty to provide excellent, compassionate, uninterrupted care, regardless of weather and climate events. This involves:
- Ensuring that facilities remain fully functional and are prepared for the best patient outcomes and experience, no matter the unforeseen circumstances.
- Providing caregivers with peace of mind, which includes knowing that your health system is equipped to handle unexpected events, and staff will remain focused on their loved one’s health.
- Empowering staff to deliver the highest quality care by fostering a safe and comfortable environment without outside distractions.
Planning for Uncertainty
Health systems must integrate resilience planning into both the design process of new facilities and the evaluation of existing facilities to successfully adapt to, respond to, and recover from weather and climate events.
Ideally, resilience planning in health systems should be an integrated workstream of master plan efforts and a health system’s overall strategic plan. Coupled together, the plans can evaluate a health system’s facilities and infrastructure as a holistic ecosystem that is aligned with a strategic vision and goals. We’ve seen that without this overarching process, health systems have sustained preventable damage from weather and climate disasters.
As designers, it is important to help our clients build better by planning for uncertain times, including:
- Storms - As strange as it may sound, preparing for a big storm like a hurricane or a blizzard is relatively easy. There is generally a window of time to coordinate a health system’s emergency plans, which includes protecting the facility and people within. The problem lies with the general lack of notification of unexpected storms. By creating resilience guidelines at the onset of the master planning process, it’s possible to minimize disruption and provide quality care for the community. For example, several health systems feature green roofs to manage stormwater runoff, and they also serve as spaces dedicated to fostering environmental and patient wellness.
- Floods - In severe storms and certain geographic areas, flooding may occur. It is essential to evaluate the critical equipment that must be elevated or relocated to remain functional. Some critical existing buildings are developing new risks as riverine flooding and cloud bursts are growing more frequent and intense. In addition to evaluating whether to wet floodproof or dry floodproof those areas at risk, health systems should also review access to facilities or be prepared to reroute patients, staff, supplies, and services.
- Energy - In high temperatures, health systems often serve as cooling centers for the community. Though the cooling centers are a much-needed resource, the added pressure on the electrical grid could cause the area to experience power outages. To alleviate this added strain and prevent overspending on generators, designers can inventory, assess, and right-size a health system’s non-critical spaces and recommend reallocation strategies of space distribution.
Case Study: A Climate Resilience Plan for NYC Health + Hospitals
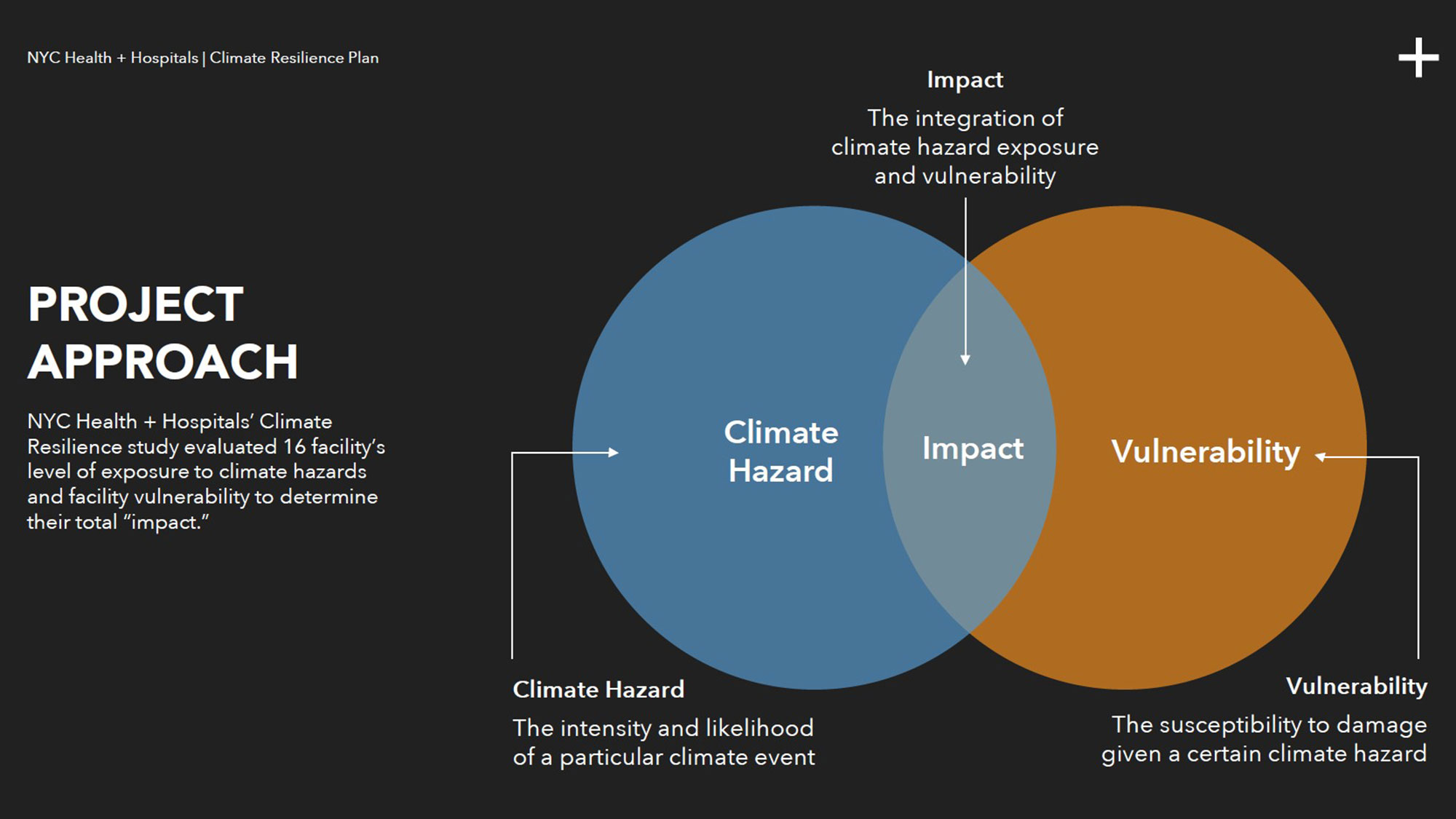
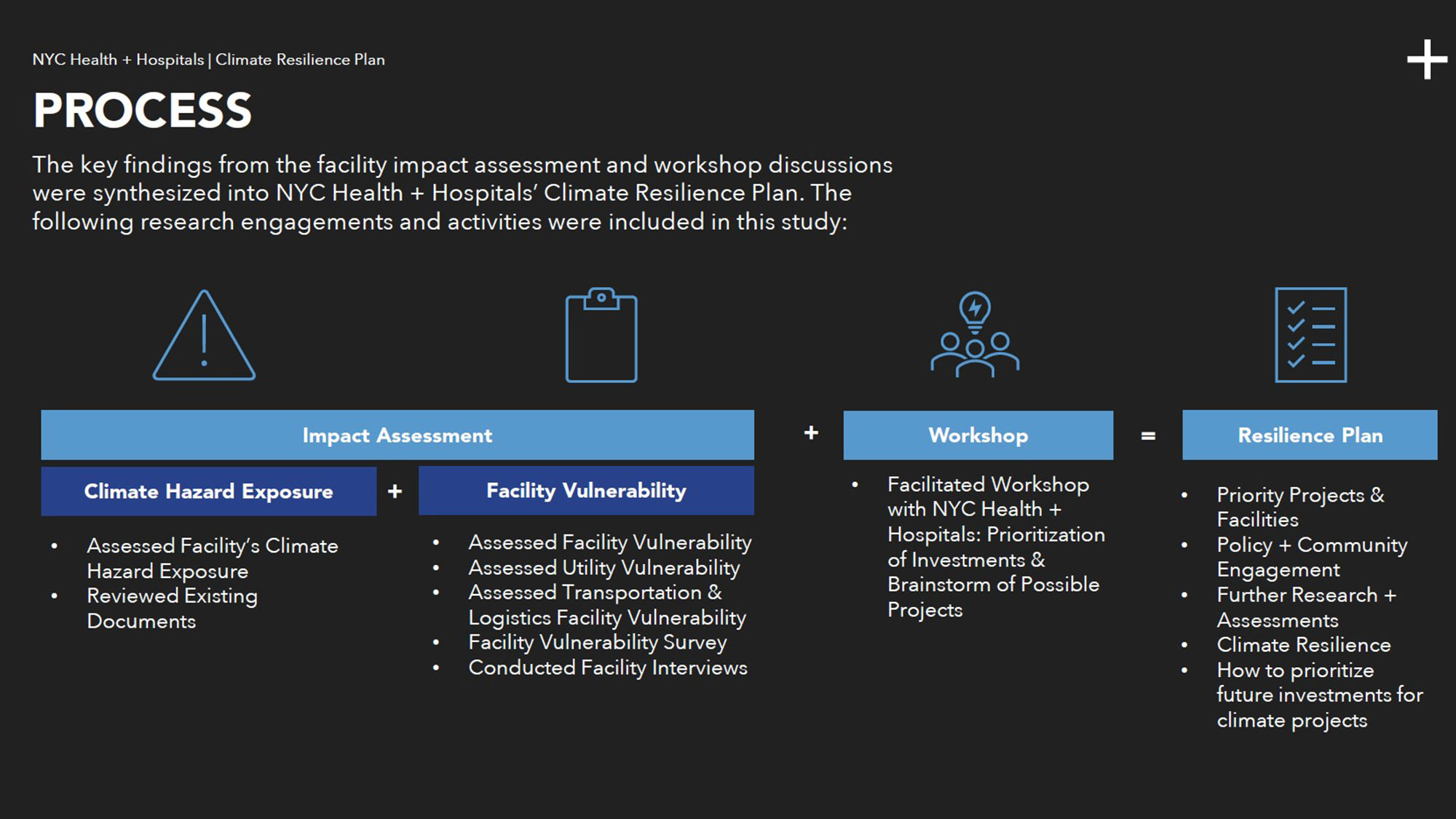
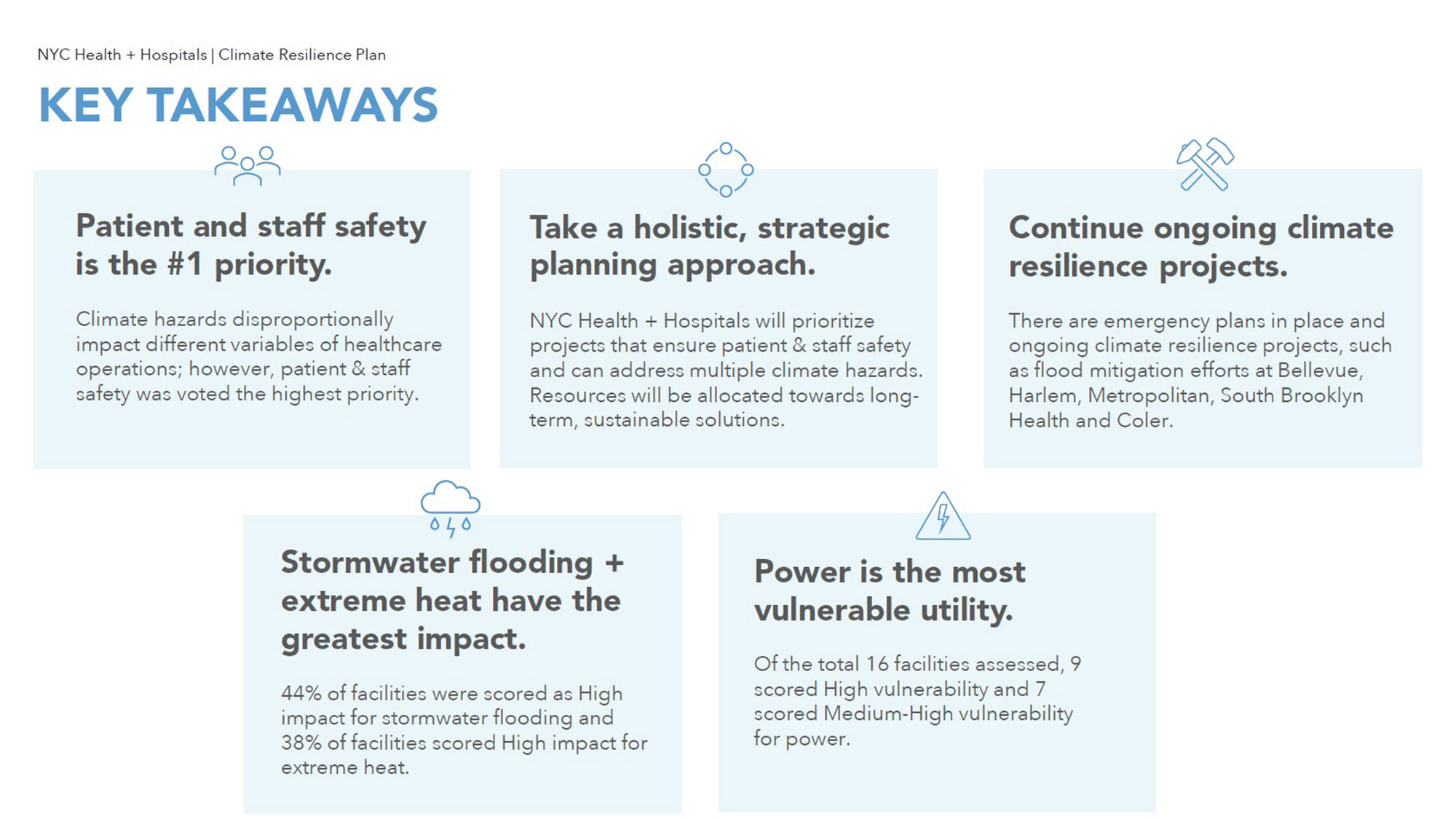
To develop a Climate Resilience Plan for the nation's largest public health care system, NYC Health + Hospitals, Gensler and Arup Engineering evaluated the resilience of 11 hospitals and five post-acute/long-term care centers.
As part of the one-year study, the team analyzed the impact of climate hazards — including stormwater flooding, coastal flooding, extreme heat, and wind — with the vulnerability of each facility. Gensler and Arup Engineering then identified potential projects and next steps to implement the Climate Resilience Plan through a series of surveys, interviews, and workshops.
Findings from the NYC Health + Hospitals Climate Resilience Plan recommended the installation of additional emergency generators linked to critical HVAC equipment, improving the drainage capacity of roofs and windows, building additional flood barriers, and installing green infrastructure to reduce ponding and heat island effect. These recommendations are in line with NYC Health + Hospitals’ commitment to the US Department of Health and Human Services Health Sector Climate Pledge and will enable the health system to continue providing uninterrupted care to the community in the future.
A Comprehensive Approach to Resilience Planning
It is equally crucial for a client to include individuals with expertise in engineering and resilience, as well as those who create and implement emergency plans and policies, within their steering committees and focus groups. Additionally, representatives from patient, caregiver, and staff experiences should be involved to provide a human-centered perspective.
Strategic and master plans should be periodically reassessed and updated to reflect the latest weather and climate projections, evolving health system policies, and changes in local jurisdiction laws and initiatives. This ensures a complete and adaptable approach to long-term planning and preparedness.
Ultimately, we must transcend the current framework for designing healthcare facilities and recognize that resilience planning is not a one-time effort based on a snapshot in time, but a continuous, collaborative process. By investing more time in proactive preparation, rather than merely reacting to challenges, we can create a healthcare ecosystem that is resilient, adaptive, and equipped to meet the evolving needs of the future.
For media inquiries, email .