The Future of Healthcare Is
Anchored in Its Communities
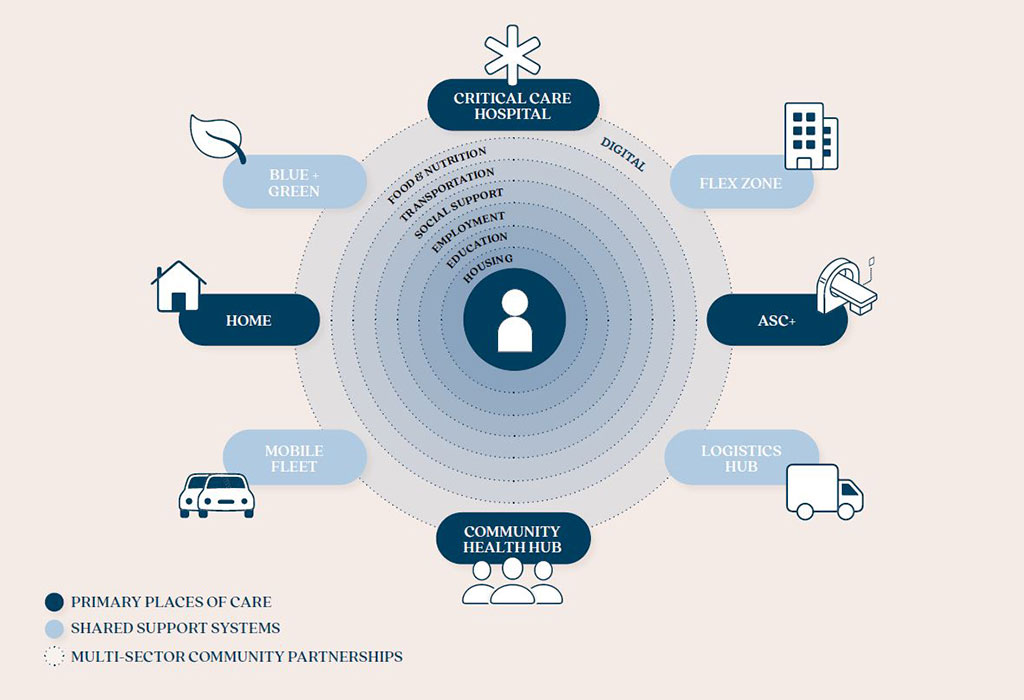
Community health hubs will play a vital role within an integrated ecosystem of health and care.

Expanding upon Gensler’s research-driven vision for the future of healthcare, this article explores the ideas behind the community health hub and its role within an integrated ecosystem of health and care.
In a future where healthcare prioritizes community health outcomes while addressing financial and workforce challenges, trust and access will be essential to success. Historically, medical services have been driven outward from hospitals, often through inequitable strategies. In contrast, Gensler’s proposed ecosystem centers health and care in a radically accessible, community-led model known as the community health hub.
The Medical Home 2.0
The community health hub represents the future anchor of both the healthcare ecosystem and communities. It combines the convenience of retail health with the premium service of concierge care and the public health strength of community health centers. These hubs shift the focus upstream, aiming to optimize health span and address leading causes of mortality, like metabolic disorders and cancer, by emphasizing prevention, early detection, and chronic illness management.
Modeled after the proven success of patient-centered medical homes, these hubs are staffed by multidisciplinary care teams that provide integrative, whole-person care. This model allows providers to manage more patients, deliver higher-quality care, and reduce costs.
Personalized Services
Each community health hub’s core service is integrative primary care for the whole family, which includes mental health, prenatal care, and lab services. Care team navigators, in partnership with local organizations, connect patients to a variety of support services addressing social, lifestyle, and environmental factors that impact health outcomes, such as nutrition, housing, job training, childcare, and transportation.
Informed by a community needs assessment, each hub may also offer services like physical therapy, dental care, pharmacy, fitness programs, and birthing services. A key element of the hub’s success is its agility — adapting its services to meet the community’s changing needs. This flexibility allows specialty services, like vision testing, cancer screenings, and diagnostic imaging, to be brought in on-demand through visiting specialists or mobile units.
Care by the Community
Trust is essential to a successful patient-provider relationship, but many communities (particularly Black Americans) have a well-founded mistrust of our traditional healthcare institutions. Understanding that trust increases when patient and provider come from similar backgrounds and have a shared contextual understanding, community health hubs are most successful when led by the specific community being served. This model also creates local jobs and strengthens social support networks. In the background, we see regional health systems and governmental agencies acting as partners for resources as needed. With leadership from within the community, these hubs can establish the trusting relationships needed for effective chronic disease management.

Radically Accessible
Access to quality healthcare is a critical social determinant of health, as healthcare providers are often concentrated around hospitals and wealthier neighborhoods. The “healthcare deserts” this creates (much like food deserts) impose additional challenges for those already facing significant barriers to care. In many urban areas, a short distance can translate into long travel times via public transit and a loss of wages for hourly workers. The community health hub offers a solution: co-located with essential services such as grocery stores, libraries, daycare centers, and schools, and accessible within 20 minutes by public transit for every urban resident.
Accessibility is not just about physical locations; it’s about removing barriers like language, health literacy, insurance coverage, hours of operation, and appointment availability. The community health hub’s integration into a broader ecosystem means patients can choose how they engage with their care team — whether in-person, virtually, at home, or through a mobile unit — depending on what works best for them.
VIP for All
Data-driven personalized medicine is no longer just a luxury for the elite. With wearable biometric devices and genomic testing becoming increasingly accessible, patients and providers can gain valuable insights that can improve health and even save lives. These technologies may have a cost, but they offer the potential to reduce overall healthcare expenses by promoting patient engagement and providing early alerts about potential health issues. At the community health hub, wearables and genomics will play a key role in democratizing healthcare, equipping both care teams and patients with the tools they need to maintain health.
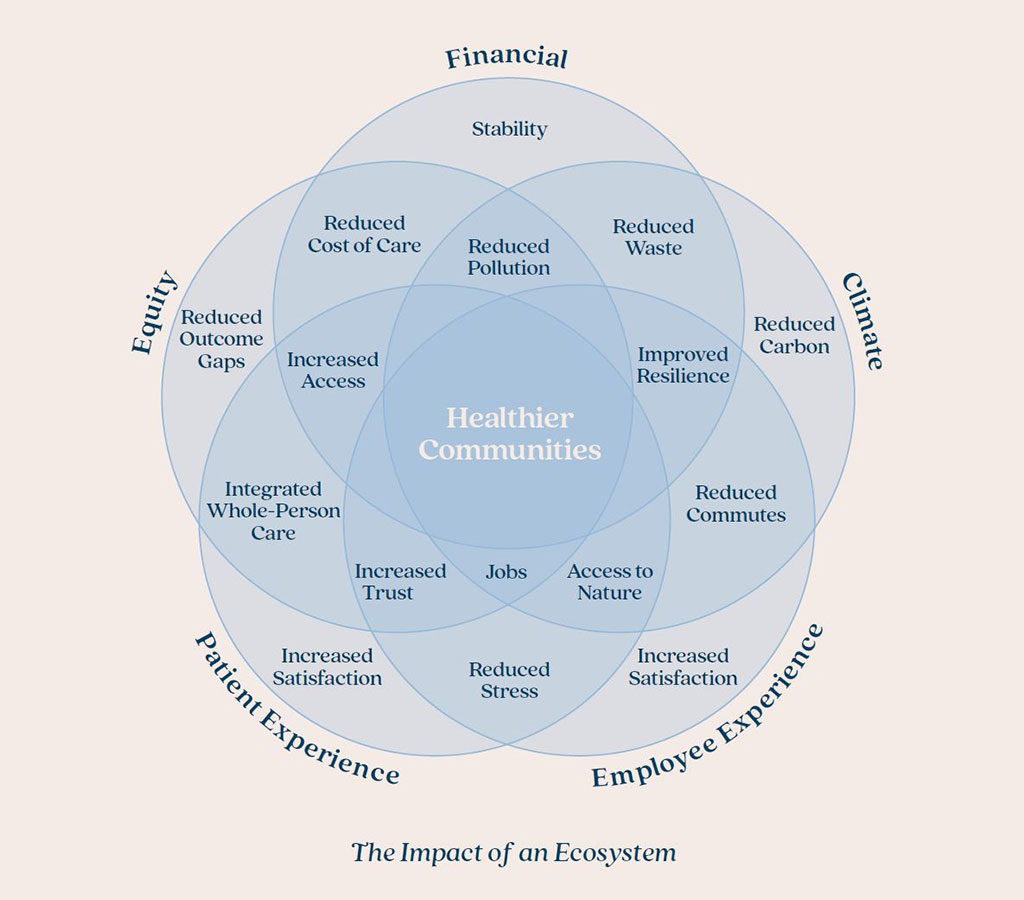
Designing for Impact
The community health hub offers the potential for the most significant, evidence-based improvements in community health outcomes. By focusing on health equity, we can narrow the life expectancy gap that has been shaped by generations of social injustice. By bringing care closer to home, we not only increase accessibility for patients but also improve work-life balance for healthcare workers, who will benefit from shorter commutes and hybrid work options. Shifting more healthcare resources upstream to prevent illness will also reduce the demand for expensive, carbon-intensive hospital care in the long run.
With community health as our guiding principle and collaboration across the healthcare ecosystem, we have an exciting opportunity to design a healthier, more equitable future.
For media inquiries, email .









