How the Rise in Digital and Home Health Will Transform Healthcare
New technologies and digital tools leveraging AI are starting to redefine how we manage our personal healthcare needs — and it starts at home.

Anyone who has ever experienced the Western healthcare system knows it can be disjointed and difficult to navigate, especially for those with multiple chronic conditions. This system is magnificently designed to treat acute illness and injury but falls short in the kind of long-term health management required to optimize health and well-being.
We see this dynamic changing with the rapid expansion of both the wellness economy and digital health industry. New technologies and digital tools leveraging AI are starting to redefine how we manage our personal healthcare needs — and it starts at home.
A new approach to home health
There are two general categories of home care. First are “hospital at home” models that allow patients to receive acute or post-acute care in the comfort of their home as opposed to the hospital. These models are centered on home care aid and remote monitoring with specific equipment, technology, and (potentially) residential accessibility renovations.
The second category can be described as “health optimization at home,” an approach with the potential to drive innovation in the industry by filling the gaps in mainstream healthcare. This new model is driven by direct-to-consumer technology, the rise of digital health practices, and AI.
Short term, this shift is satisfying unmet patient demand for more advanced, personalized primary and specialty care, including access to cutting-edge diagnostics. It emphasizes virtual-first, person-directed care.
Long term, the innovative ideas behind these disruptive technologies and care models have the potential to change mainstream best practices, shift more care upstream, reduce the need for downstream interventions like surgery and even the demand for hospital beds, and increase both lifespan and healthspan.


The role of AI, remote monitoring, and virtual technologies
A key driver that is facilitating this shift to upstream prevention and prediction is the advancement of new and more accessible technology.
Wearable smart devices can track vitals and detect health risks — and provide early alerts — before these risks progress into serious conditions. The data gathered from your Apple Watch or Oura Ring can be monitored by AI and a provider on the back end to deliver precision health recommendations based on your personal goals.
Whether your focus is on longevity, weight loss, mental health, or chronic disease management, this technology is becoming a vital tool in conversations between patient and provider, guiding personalized plans for testing, lifestyle interventions, supplements and medications, and other interventions.
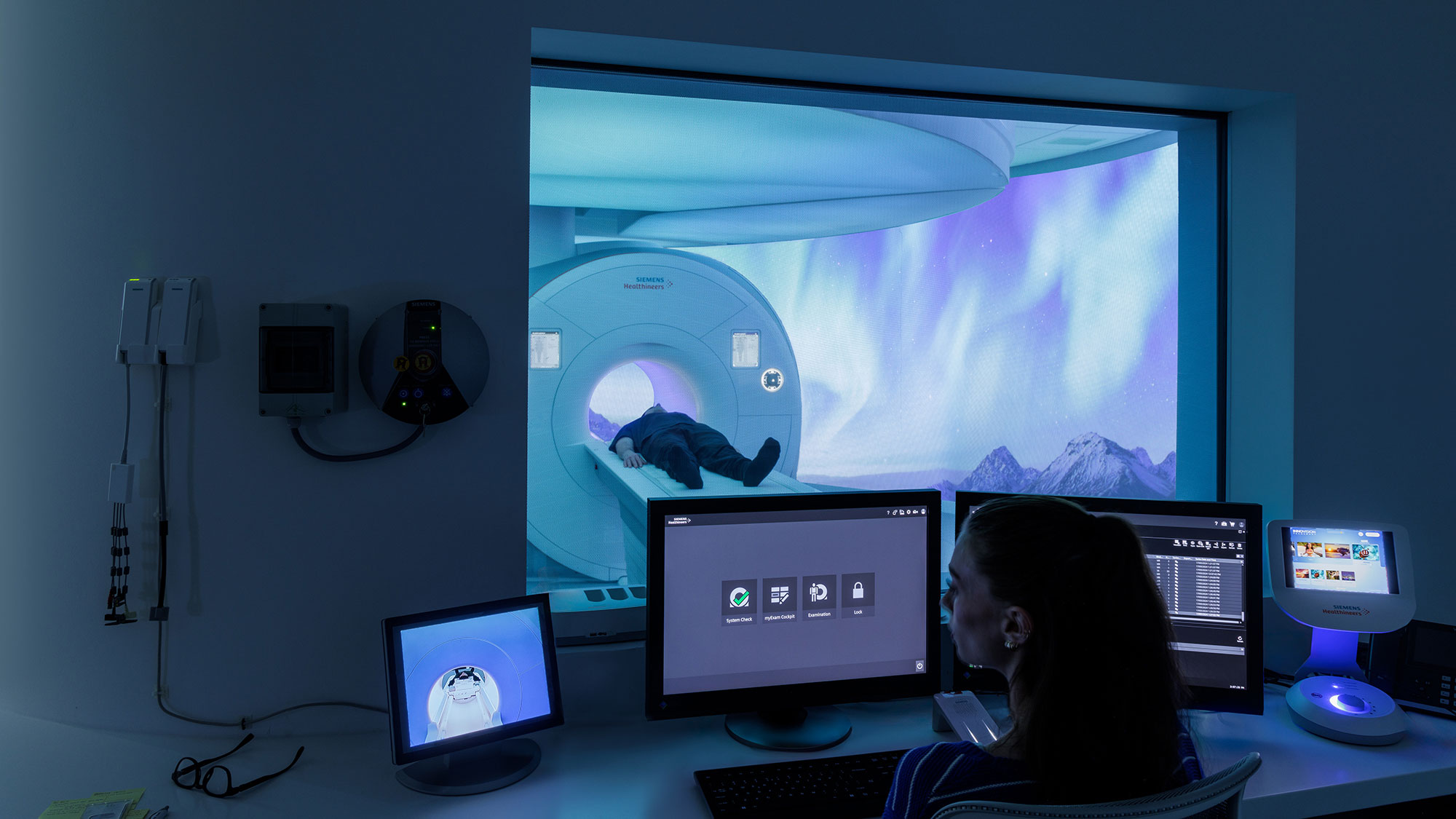
The next generation of technology includes medical devices that may soon replace bulky, standard radiological equipment. Skin scanning apps, ECG apps, handheld ultrasound, and more are starting to redefine portable diagnostics. Given the high cost and dedicated spaces required to support current equipment, these technologies could also reduce overall expenditures.
Increasingly, AI is also able to connect the dots between disparate data points and provide deeper insights. In the not-so-distant future, we’ll see AI analyzing the biomarker data gathered by multiple digital health sensors, from your smart watch to your smart scale and even your smart toilet, to make more accurate diagnoses than current modalities.
Telehealth is another key feature of this health at home model. The pandemic accelerated virtual doctor’s visits, and it appears that the practice is here to stay. According to the American Medical Association (AMA), 74.5% of physicians work in practices that offer telehealth — up from just over 10% in 2018.
Telemedicine is crucial for people who live in rural or remote areas. The Association of American Medical Colleges (AAMC) says the average wait time for a new patient appointment with a specialist in rural areas can range from 30 to 45 days, depending on the specialty and region. With virtual-first care, patients can access specialists for health concerns ranging from hormonal health to metabolic wellness without waiting months for an appointment for an in-person visit or traveling long distances.

Care delivered to your door
With expanded at-home diagnostic and testing capabilities, blood collection that used to require a phlebotomist can be done at home, with everything from micronutrient panels to cancer screening kits mailed to your door.
With increased drone deliveries of medications and supplies from companies like Amazon Pharmacy to providers like Mayo Clinic and Cleveland Clinic, we’re likely to see a shift towards fewer traditional retail pharmacies and a rise in centralized pharmacy warehouses, as drones can efficiently deliver from these warehouses directly to patients’ homes.
This could help bridge the gap in healthcare access, particularly in remote or rural areas, where pharmacies may be inaccessible. We could also see fewer walk-in clinics as care is delivered directly to patients’ homes. Long term, advancements in biomarker testing for conditions like cancer could change standards for routine screening, replacing traditional mammograms and colonoscopies.

Design implications
The design implications for this new approach to medical care are significant. Healthcare design is already evolving away from a one-size-fits-all approach, so this type of virtual/physical hybrid model at home would accelerate the demand for personalized and specialized medicine even more.
User-centered experience design is key — patients expect seamless digital interactions. For example, a medical digital twin — a virtual, dynamic representation of a patient’s health, built from their medical records, real-time data from wearables, medical imaging, and other sources — has the potential to provide more personalized and predictive healthcare and potentially lead to earlier interventions and better health outcomes.
Also, as patients become more informed and savvy consumers, they will seek out curated, subscription-based healthcare services that align with their personal brand and specific health needs.
Already, we’re seeing companies like Neko Health and TELUS Health provide such services – and they’re more than a digital-only experience. They offer experiential, hospitality-driven physical destinations akin to a luxe spa or wellness experience.
As designers, we have an opportunity to create a branded physical-digital patient journey that includes at-home healthcare products and hospitality like in-person destinations.
The role of community health hubs
We also believe that community health hubs will play a vital role in this new upstream model of care.
Right now, few of these at-home solutions are covered by insurance. They are primarily available to those with the financial means to pay out of pocket and are presently increasing the health equity gap. But what if monitoring or screening tools were available more broadly?
At community health hubs, we see wearables and genomics playing key roles in democratizing healthcare, equipping both care teams and patients with the tools they need to optimize health.
These physical spaces can act as check-in points when needed, but most care can take place remotely and in-home. As a result, healthcare shifts from a disjointed collection of providers and facilities to a coordinated, integrated, community network of care.
The most effective healthcare system is one that prevents illness before it starts. We believe that a preventative, wellness-driven model is transforming healthcare. Technology, digital design, and infrastructure support are key to making this shift sustainable. But it’s also critical to balance efficiency with a human-centered approach.
The future of healthcare is proactive — it’s about helping people stay well and expand their health spans and their quality of life, rather than just treating illness.
For media inquiries, email .